Two years ago, cases of the infectious viral disease mpox were rising rapidly in cities around the world, particularly in the United States, prompting a scramble to secure vaccine doses to help contain the outbreak and ease the uncomfortable symptoms of the virus.
That strain of mpox was rarely fatal, but authorities soon declared it a global public health emergency in July 2022. In the months that followed, the spread of the virus steadily declined, though cases never completely disappeared.
But last week, a much more worrying variant of the monkeypox virus, formerly called monkeypox, has once again prompted a global health alert. This outbreak is primarily affecting countries in central Africa, but authorities warn that it appears to spread more easily than the 2022 strain and is significantly more deadly.
Where is mpox a concern right now?
The World Health Organization has deemed this clade, or variant, of the mpox virus to be the latest global health emergency. Most of these mpox virus clade I cases have been reported in the Democratic Republic of the Congo, where there have already been 14,000 cases and 524 deaths this year, according to Tedros Adhanom Ghebreyesus, director-general of the World Health Organization.
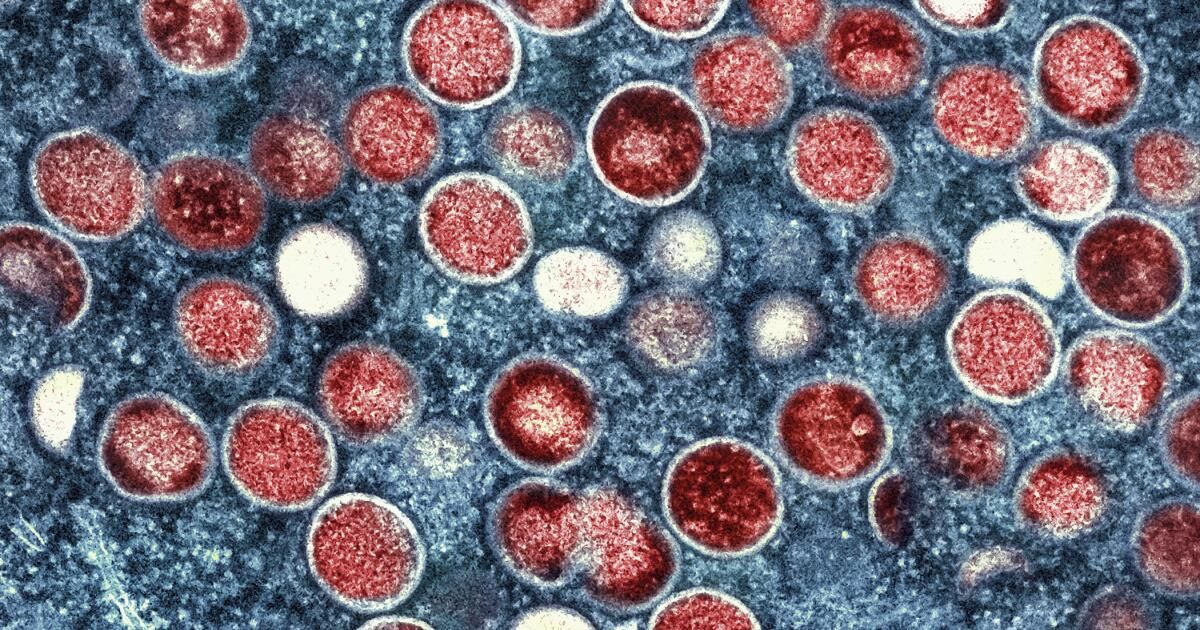
Mpox belongs to the same family of viruses as smallpox, but causes milder symptoms, such as fever, chills, and body aches. People with more severe cases may develop lesions on their face, hands, and chest. With recent Mpox outbreaks, lesions can also develop on a person's genitals, which can make it harder to detect and, in turn, easier to spread.
While this virus is endemic, or naturally occurring, in Congo and parts of central Africa, health authorities have also recently detected this more worrisome strain in other nearby non-endemic countries, with the first case confirmed outside Africa in Sweden. Public health officials are concerned about the “possibility of further spread to other countries in Africa and possibly beyond the continent,” according to the World Health Organization.
As of this summer, the CDC still considers the risk of mpox to the general public in the U.S. to be very low, but said the risk is slightly higher among men who have sex with men. During the global mpox outbreak in 2022, gay and bisexual men made up the vast majority of cases, as the virus spread primarily through close contact, including sexual intercourse.
Some of those patterns have been seen in the new outbreak in Central Africa, but officials have said that children under 15 now account for more than 70% of mpox cases and 85% of deaths in Congo.
It's important to note, however, that there have been no confirmed cases of the new mpox variant in the U.S. and health officials say they are closely monitoring the situation.
Should Californians be worried?
The 2022 outbreak “should have made clear that infectious diseases do not respect borders and that what happens in one part of the world can quickly become a concern for all,” said Dr. Anne Rimoin, a professor of epidemiology at UCLA.
And while the risk of widespread transmission outside Africa is very low, he said public health officials should not become complacent.
“That said, as I always say, an infection anywhere is potentially an infection everywhere,” Rimoin said, “and our best chance of reducing the impact of Clade I-related infections is early detection and response.”
But Californians shouldn’t stress about transmission of this latest strain because “we have the tools to be able to control mpox through surveillance, testing, case management, vaccinations and public health messaging,” she said.
What are local officials doing?
The 2022 variant, known as Clade II, continues to circulate in the United States, including in Los Angeles and San Francisco, two of the epicenters of the latest outbreak.
“We see intermittent detections of Clade II in our wastewater,” said Dr. Julia Janssen, deputy director of the HIV/STI Prevention and Control Division at the San Francisco Department of Public Health. “It’s not cause for alarm.”
So far this year, San Francisco has seen about one case per week. Los Angeles has seen a slight increase in cases this summer.
“We continue to monitor mpox development along with our state and federal partners,” Janssen said. He noted that there is now a robust testing infrastructure, unlike during the last mpox outbreak, that will help identify when and if the clade I strain reaches the U.S.
The recent declaration of an international health emergency puts countries, including the United States, on alert to improve surveillance and detection, Rimoin said.
This month, the California Department of Health issued an advisory to health care providers warning “of an increased index of suspicion for Clade I mpox in patients who have recently traveled to Africa and present with signs and symptoms consistent with mpox.”
The recent health emergency declarations will also unlock resources that would otherwise be unavailable for global coordination, critical research to address knowledge gaps and public health response, Rimoin said.
It also helps that this is not a completely new virus, he said. The key to containment is early detection and response.
What should you do, if anything?
“We continue to strongly recommend and encourage two-dose vaccination” for those considered at higher risk, Janssen said. He noted that only certain groups of people fall under the vaccination recommendations, because the risk to the general public remains low. The CDC continues to recommend that anyone exposed to mpox get vaccinated, as well as certain gay, bisexual or other men who have sex with men.
Despite the geographic location of the new outbreak, Janssen said there is “no travel-only vaccination recommendation.”
The Los Angeles County Department of Public Health continues to recommend that people who should get vaccinated are:
- Men or transgender people who have sex with men or transgender people.
- People of any gender or sexual orientation who engage in commercial and/or transactional sex.
- People living with HIV, especially people with uncontrolled or advanced HIV disease.
- People who have had skin-to-skin contact or intimate contact with someone with suspected or confirmed mpox, including those who have not yet been confirmed by the public health department.
Are there vaccines and/or treatments available to prevent MPOX?
Yes. The good news is that there are plenty of doses of the Jynneos vaccine, which is used to prevent both smallpox and mumps.
CDC officials have said that “medical countermeasures that have been effective for clade II mpox are also expected to be effective for clade I mpox,” Janssen said. “That includes Jynneos, the vaccine that has been recommended … as well as other treatments.”
At this time, the mpox vaccine is free across the United States and in California. The Los Angeles County Department of Public Health is providing the 2-dose JYNNEOS vaccine. The county has a Online list of vaccination sites where the mpox vaccine is offered.
If I was vaccinated two years ago, should I get a booster dose?
Booster vaccinations are not currently recommended.
“People who have completed the series do not need to receive additional doses,” Janssen said. “And people who have already been infected do not need to be vaccinated.”