The history of medical diagnosis is a march through careful observation. Ancient Egyptian physicians first diagnosed urinary tract infections by observing patterns in patients' urine. To diagnose heart and lung diseases, medieval physicians added basic elements of the physical examination: pulse, palpation and percussion. The 20th century saw the introduction of laboratory studies, and the 21st century the sophistication of imaging and genetics.
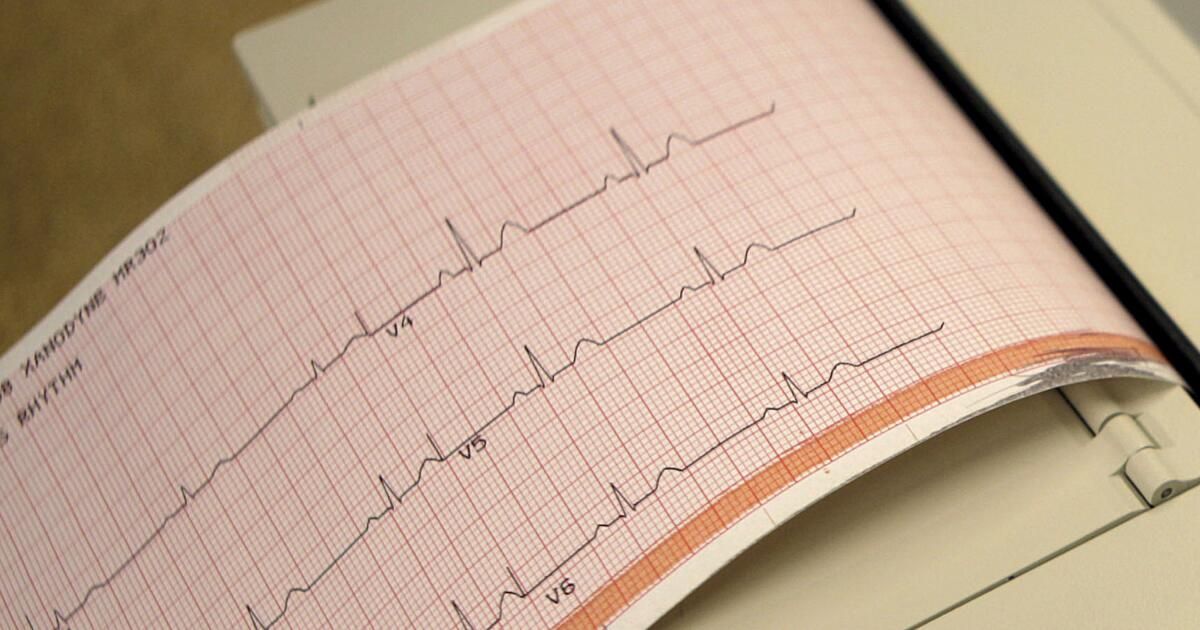
Yet despite advances, diagnosis remains largely a human endeavor, with doctors relying on so-called disease scripts — sets of signs, symptoms and diagnostic findings that are the hallmarks of a disease. Medical students spend years memorizing such scripts and are trained to, for example, identify the submillimeter variations in electrocardiogram wave measurements that might alert them to a heart attack.
But humans, of course, make mistakes. Sometimes, misdiagnosis occurs because a doctor misses something: when disease patterns fit the script, but the script is misinterpreted. This happens over an estimated period of 2010. 15% to 20% Other times, misdiagnosis occurs because the disease has features that don't match known patterns—that is, they don't fit the script, such as when a heart attack occurs without telltale symptoms or ECG findings.
Artificial intelligence can help solve both of these fundamental problems, if given sufficient financial support and implemented correctly.
First, AI is less susceptible to the common factors that lead doctors to make diagnostic errors: fatigue, Lack of time and cognitive bandwidth when treating many patientslagoons of knowledge and confidence in mental shortcutsEven when diseases fit scripts, computers will sometimes be better than humans at identifying hidden details in voluminous health data.
Using AI to improve the accuracy and timeliness with which doctors recognize diseases can mean the difference between life and death. Ischemic stroke, for example, is a life-threatening emergency in which a blocked artery prevents blood flow to the brain. Brain imaging confirms the diagnosis, but those images must be quickly and accurately taken and interpreted by a radiologist. Studies show that AI, thanks to superhuman pattern-matching capabilities, can identify strokes within seconds of the images being taken. Tens of minutes before radiologists, who are often very busy. Similar capabilities have been demonstrated in the diagnosis septicemia, pneumoniablood clot in the lungs (pulmonary embolism), Acute kidney injury and other conditions.
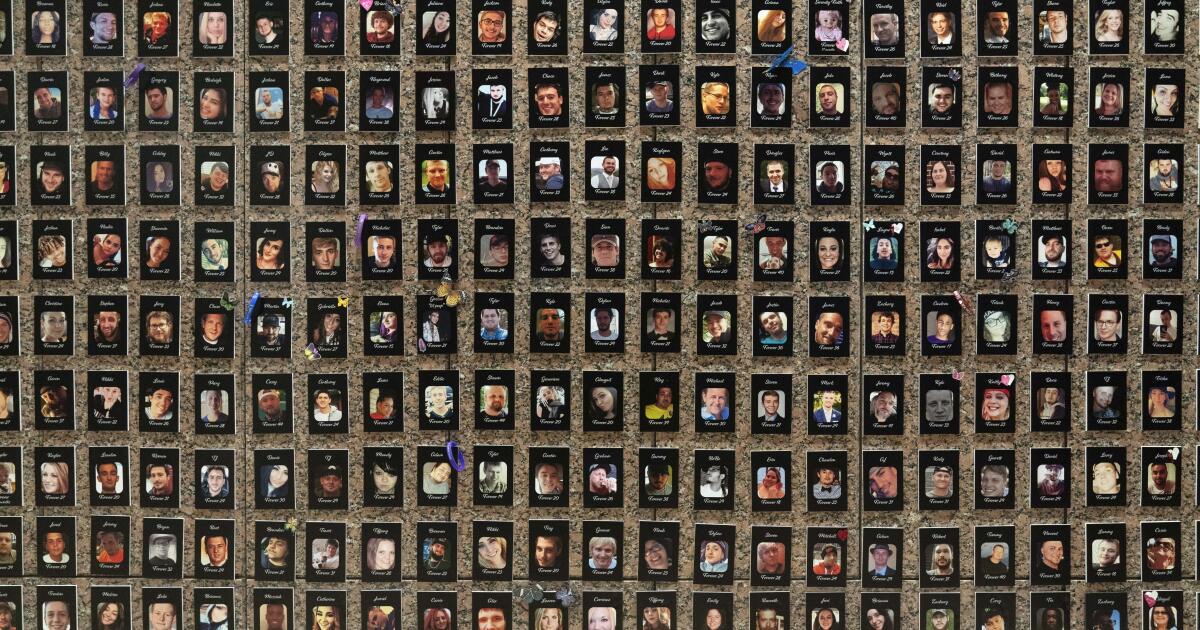
Second, computers can be useful for diseases for which we have not developed the appropriate scripts. AI can, in fact, diagnose diseases using new patterns too subtle for humans to identify. Consider, for example, hypertrophic cardiomyopathy, a rare genetic disease in which the heart muscle has grown larger than it should, leading to heart failure and sometimes death. Experts estimate that Only 20% of those affected are diagnoseda process that requires consultation with a cardiologist, cardiac ultrasound, and often genetic testing. So what happens to the remaining 80%?
Researchers from around the country, including those from the Mayo Clinic and UC San Francisco have shown that AI can detect complex, previously unrecognized patterns to identify patients likely to have hypertrophic cardiomyopathy, meaning AI-powered algorithms will be able to detect the condition in routine electrocardiograms.
AI was able to recognize these patterns after examining the ECGs of many people with and without the disease. The rapid growth of healthcare data (including detailed electronic medical records, imaging, genomic data, biometric data, and behavioral data) combined with advances in artificial intelligence technology has created a huge opportunity. Because of its unique ability to identify patterns from data, AI has helped radiologists to Find hidden cancerspathologists to characterize liver fibrosis and ophthalmologists to detect retinal diseases.
One challenge is that AI is expensive, requiring large-scale data to train computer algorithms and the technology to do so. As these resources become more ubiquitous, that can make the associated costs higher. intellectual property They are difficult to protect, which discourages private investment in these products. More generally, diagnostics have long been considered unattractive investments. Unlike their therapeutic counterparts, which spend around $300 billion on research and development, investment A year, diagnoses receive a modest 10 billion dollars in private financing.
There’s also the question of who pays for the use of AI-based tools in medicine specifically. Some applications, such as stroke detection, save insurers money (by avoiding costly ICU stays and subsequent rehabilitation). These technologies tend to be reimbursed more quickly. But other AI solutions, such as detecting hypertrophic cardiomyopathy, can lead to increased spending on costly downstream therapies to treat newly identified chronic diseases. While using AI can improve the quality of care and long-term outcomes in those cases, without financial incentives for insurers, reimbursement and therefore adoption can be slow.
Life sciences companies have rarely agreed to subsidize Developing or reimbursing AI-based diagnostics will help close the gap, but the federal government may have to play a bigger role. Support for COVID diagnosis During the pandemic, the rapid development of critical tests and the Moonshot project against cancer were promoted. Has helped boost R&D in detection and new treatments.
It is generally difficult to raise funding on the scale needed for new medical frontiers, but the National Academies of Medicine have My dear that tens of billions of dollars could be saved and countless lives could be saved by improving diagnostics in medicine.
Artificial intelligence offers a path toward that goal. It should complement, rather than replace, the human expertise that already saves so many lives. The future of medical diagnosis doesn’t mean handing the keys to AI, but rather, taking advantage of what it can do that we can’t. This could be a special moment for diagnostics — if we invest enough and get it right.
Gaurav Singal is a computer scientist and physician at Harvard Medical School. and He was previously chief data officer at Foundation Medicine, a cancer diagnostics company. Anupam B. Jena is an economist, physician, and professor at Harvard Medical School and co-author of “Random acts of medicine: the hidden forces that influence doctors, impact patients, and shape our health” and the Subpile of random acts of medicine.