California hospitals are increasingly busy with more COVID-19 and flu patients, some of whom are suffering from both viruses at the same time.
Co-occurring illness is another complication in an already hectic respiratory virus season. Although hospitals are not as full as during the emergency phase of the pandemic, they are becoming more so: Los Angeles County recently entered the “medium” COVID-19 hospitalization category described by the Centers for Disease Control and Prevention. the US Disease Prevention for the first time. time this winter.
“Some of these patients test positive for more than one virus; the flu definitely likes to travel with COVID. [And] we are seeing an outbreak of RSV,” said Dr. Daisy Dodd, an infectious disease specialist at Kaiser Permanente Southern California.
The viral cocktail could also include coronavirus or flu with RSV, or respiratory syncytial virus, simultaneously. Sometimes a common cold virus, such as rhinovirus, is in the mix.
And it’s not just the very young and the very old who are hit by a double whammy of illness: younger and middle-aged adults have been affected as well. Dodd said she has seen some patients report fevers that last more than a week.
“Now it seems like everyone has this dry cough that doesn’t want to go away,” he said. “It’s making them quite sick and… it’s not very gentle.”
For many of the patients who need medical care, “they feel miserable. No doubt about that.”
It’s hard to say why doctors are seeing so many viral co-infections this winter, experts say.
“Does one lower their immunity and allow them to catch the other easily? “I don’t know the answer,” Dodd said. “But we’re seeing a lot of ‘double whammys’ out there.”
Los Angeles County’s entry into the “medium” COVID-19 hospitalization category has prompted local public health officials to order hospitals, nursing homes and any other inpatient facilities to require hospital employees healthcare providers wear masks while in patient care areas. Visitors to those facilities must also wear masks in the same areas.
As a county enters the “medium” level of COVID-19 hospitalization, those at high risk for severe illness should wear a high-quality mask, such as a KF94, KN95, or N95 mask, when indoors and in public, the county says. CDC.
The agency also says those who live or have social contact with someone at high risk should consider getting a rapid COVID test before meeting that person and consider wearing a mask when meeting them indoors.
A negative result from a rapid COVID test helps reduce, but does not completely eliminate, the risk of transmitting a coronavirus infection. There is a chance that a single rapid test may not detect an infection in its early stages.
Performing multiple tests over a period of time, such as two or three days, can be helpful, “especially when people using them do not have symptoms of COVID-19,” according to the U.S. Food and Drug Administration.
More and more infected people are being admitted to California hospitals. During the week ending Dec. 23, 3,279 coronavirus-positive patients were newly admitted statewide, up 14% from the previous week and the highest weekly count in 10 months.
However, new hospitalizations remain considerably lower than last winter’s peak. And several hospitals are seeing no signs of a COVID-19 surge in their intensive care units.
“Our ICUs are busy, but not overwhelmed by COVID,” said Dr. Tevan Ovsepyan, medical director of the hospital program at Providence Holy Cross Medical Center in Mission Hills.
Still, the disease season continues apace. California’s level of flu-like activity, which includes non-flu illnesses like COVID-19, recently increased to “very high,” one of the worst levels as defined by the CDC, for the first time this winter.
Ovsepyan said that at his hospital there was an increase in the number of coronavirus patients about a week and a half ago that gradually decreased starting Friday. But he said: “I don’t know what the future holds, because… we have New Year’s… and people are gathering. So I’m sure we’ll probably see a little bit of an uptick.”
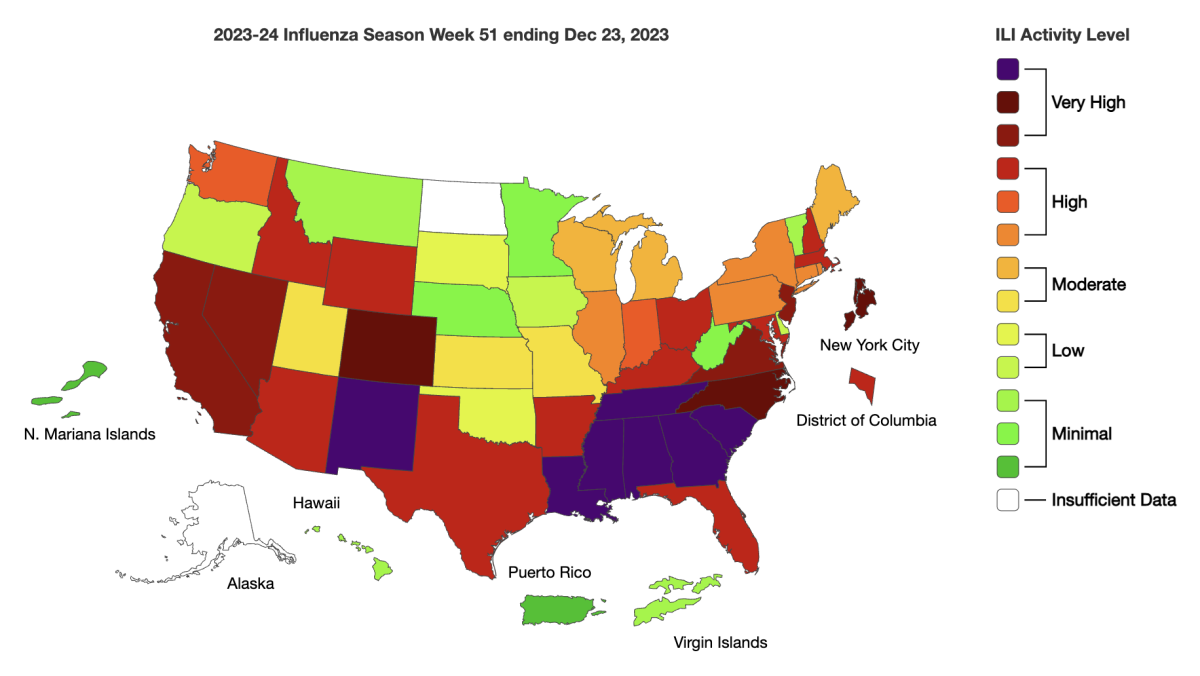
During the week ending Dec. 23, California had a “very high” level of flu-like activity, including non-flu illnesses like COVID-19, according to the U.S. Centers for Disease Control and Prevention. USA
(US Centers for Disease Control and Prevention)
Other areas of California that are in the CDC’s “medium” COVID-19 hospitalization category include the four-county area around the state capital (Sacramento, Placer, Yolo and El Dorado counties) and several counties in the rural north: Butte, Tehama and Glenn.
The rate at which lab samples test positive for the coronavirus and flu continues to increase in Los Angeles County. During the week ending December 23, the most recent available, 23% of samples tested in surveillance laboratories tested positive for the flu, a jump from the previous rate of 18%. Regarding COVID-19, 12% of samples test positive for coronavirus, an increase from 11% the previous week.
RSV, which can cause serious illness and death, especially among infants and seniors, has plateaued at a high rate across the county, with 10% of samples testing positive over the most recent week. The rate of positive tests has remained between 10% and 15% in recent weeks, a relatively high rate compared to the previous six years, but still below last year’s terrible RSV season, when the rate of positive tests exceeded 20%.
During the week ending Dec. 4, Los Angeles County averaged five COVID-19 deaths per day, up from an average of two in mid-November, though still below last year’s numbers.
In terms of serious illnesses and deaths, hospitals are in better shape than the terrible first winter of the pandemic and the initial wave of Omicron the following year.
“Omicron was just horrible. It was a terrible time, because then we were overwhelmed by COVID positives and people were sick,” said Ovsepyan, who is also president of the department of hospital medicine at Facey Medical Group, which has outpatient clinics in San Fernando, Santa Valles. Clarita and Simi.
Ovsepyan urged people to be responsible and stay home if they are sick.
And if you must leave the house and go anywhere where there is a crowd and you have symptoms like a cold, “wear a mask,” Ovsepyan said.
“Over time, people have had this COVID fatigue and mask fatigue. “All this is reasonable,” Ovsepyan said. “But it is still a virus. It still causes diseases. “It will be detrimental to our frail patients, our elderly or people with comorbidity diagnoses…those are the people who end up being hospitalized.”
Initially, people may ignore a small cold or a small sore throat. But that can be the start of a full-blown viral illness, and it would be “fabulous” if those who feel that way start wearing a mask as soon as possible to protect those around them, Dodd said.
“Probably 95%, if not more, of respiratory infections are felt in the throat to begin with,” he said.
It is likely a combination of factors that have led COVID-19 to be less deadly than it used to be, including the protection provided by vaccines and persistent immunity against infection, as well as the development of anti-COVID drugs. that can be taken after infection.
But health officials are concerned about the lackluster use of these drugs, as well as the delay in adoption of the latest COVID vaccines. The CDC urges virtually everyone over 6 months of age to get a new COVID-19 vaccine this winter, as well as the seasonal flu vaccine.
RSV vaccines are also available for infants, pregnant women, and people age 60 and older.
Authorities are urging more widespread use of antiviral drugs like Paxlovid, which can reduce the severity of symptoms and the risk of hospitalization and death. It’s best to take them right from the start, but many people don’t or their healthcare providers don’t prescribe them.
“There is an ample supply of therapeutic agents for COVID-19, but they have been underutilized,” the California Department of Public Health said in a health advisory. “Unfamiliarity with new medications… and misperception of drug shortages have contributed to low treatment rates, including reports of eligible patients ultimately being denied treatment.”
California still offers a free telehealth service through Sesame Care, where sick people can talk to a health care provider by phone or online and get a prescription, if they are eligible. (A co-payment may be required to pick up the prescription.) That service is available to Californians ages 12 and older, regardless of insurance status, through February by calling (833) 686-5051 or visiting sesamecare.com/covidca.
Los Angeles County residents can do the same by contacting the county’s public health call center at (833) 540-0473, which is open seven days a week, 8 a.m. to 8 p.m. The county says free and low-cost treatment is available for eligible patients. , including those who are uninsured or on Medi-Cal.
A program funded by the National Institutes of Health, presented in test2treat.org, provides adults who test positive for COVID-19 or flu free access to telehealth care and treatment. That program is expected to run through early summer. Adults who do not test positive can still sign up for free testing if they are uninsured or underinsured; on Medicare or Medi-Cal; or in the health system of the Department of Veterans Affairs or the Indian Health Service.
The US government is also allowing residents to request free at-home COVID tests through TestCovid.org. People can request four free home tests per household. And if you haven’t already placed an order between September 25 and November 19, you are eligible for two separate orders of four tests.












