The commercials make it sound very simple: “If it's COVID, Paxlovid.”
But the slogan, catchy as it is, belies a harsher reality that some elected and public health officials have long recognized and worked to rectify: For many, gaining access to therapy should be much easier than it has been. been.
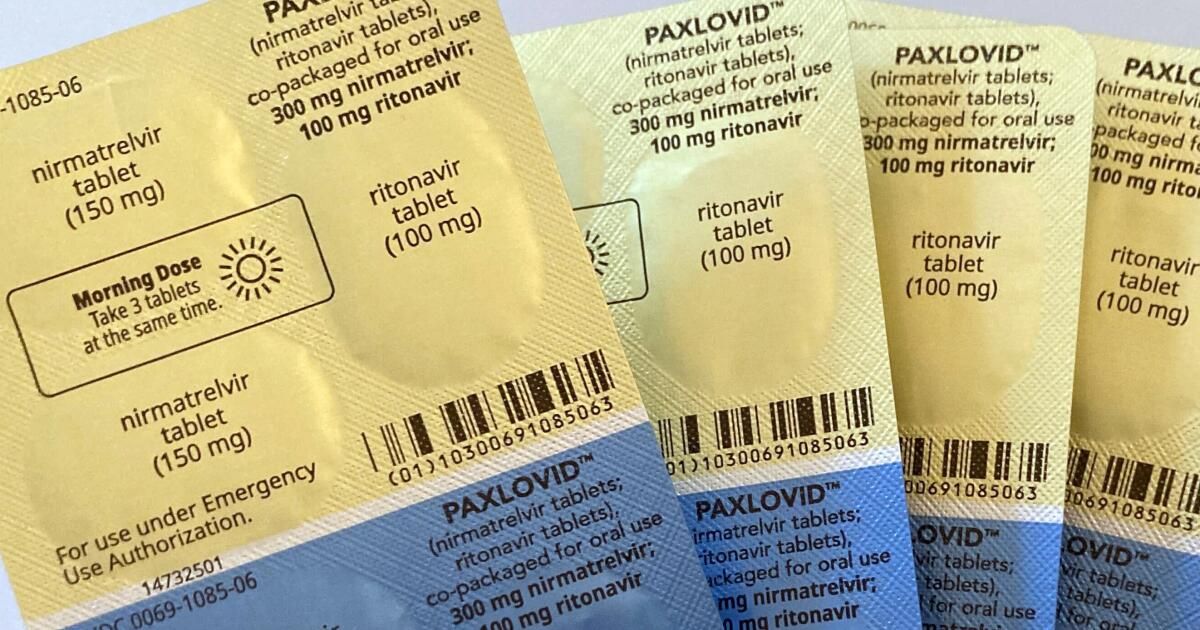
The problem is not one of scarcity, since the antiviral is abundant. Price is also not a major barrier, as Paxlovid is cheap or even free for many. It's not even a question of how well it works, as studies have shown it to be very effective.
The drug's biggest impediment has been, and continues to be, the simple fact that several doctors still refuse to prescribe it.
Some healthcare providers base their reluctance on outdated arguments, such as the idea of the “Paxlovid rebound”: the possibility that people taking the drug have a chance of developing COVID symptoms again, usually between two and eight days after recuperate.
It turns out that anyone who contracts COVID-19 has a similar chance of recovering.
COVID rebound “can occur with or without [Paxlovid] treatment,” Food and Drug Administration scientists wrote in a study published in December. “The rebound of viral RNA was not limited to [Paxlovid] “Recipients and rebound rates were generally similar to placebo recipients.”
When told about a patient who was denied a prescription for Paxlovid due to concerns about “Paxlovid rebound,” Dr. Peter Chin-Hong, an infectious disease expert at UC San Francisco, complained.
“Oh my God, that's so fake,” Chin-Hong said. “Doctors who have this strange idea about rebounds, it's just nonsense.”
The data indicates that most people do not experience a COVID rebound, Chin-Hong said. And while rebound can occur, the possibility should not deter people “who might really need it” from taking an antiviral.
Even if a COVID rebound occurs and symptoms occur, “they tend to be mild and do not require repeat treatment,” according to the California Department of Public Health.
Officials at both the federal and state levels have implored healthcare providers to appropriately prescribe Paxlovid and other antivirals when indicated.
“Antivirals are underused,” the Centers for Disease Control and Prevention said in a statement Thursday. “Don't wait for symptoms to get worse.”
In its own notice, the California Department of Public Health said: “Most adults and some children with symptomatic COVID-19 are eligible to receive treatments…Providers must have a low threshold for prescribing COVID-19 therapies.” 19″.
Aside from Paxlovid, an alternative oral antiviral treatment is known as molnupiravir. There is also remdesivir, which is administered intravenously.
The CDC says Paxlovid and remdesivir are the preferred treatments for eligible COVID-19 patients.
“Don't delay: Treatment should be started within five to seven days of when symptoms first develop,” the CDC says.
A reference to Paxlovid and other antivirals even appears in a musical radio advertisement by California health authorities that has been broadcast throughout the state: “Try it. Treat it. You can beat it,” and the song continues later: “Medication is key / To stop the virus in your body.”
However, there is extensive documentation of the low frequency of prescription of Paxlovid and other antivirals, and this may have significant consequences for higher-risk COVID-19 patients. A report released by the CDC on Thursday reviewed 110 COVID-19 patients considered high risk and found that 80% of them were not offered antiviral treatment.
A major reason given by the patients' providers, all of them under the Veterans Health Administration, was that their patients' COVID symptoms were mild.
But, as officials point out, that's exactly what antivirals are for.
“There is strong scientific evidence that antiviral treatment of people with mild to moderate illness, who are at risk for severe COVID-19, reduces their risk of hospitalization and death,” the CDC says.
Risk factors for severe COVID-19 include being 50 years or older; not being up to date on COVID vaccines; and a wide range of medical conditions, such as diabetes, asthma, kidney disease, heart disease, anxiety or depression, and being overweight. Other factors that influence health, such as limited access to health care and low income, can also increase a person's risk.
Another reason providers may cite not prescribing COVID antivirals, California officials said, is the possibility of serious side effects. But that fear is largely misguided, since “most people have few or no side effects,” says the California Department of Public Health. Some of the most common side effects after taking Paxlovid are the development of a temporary metallic taste in the mouth, which occurs in approximately 6% of recipients, and diarrhea (3%).
However, some people taking Paxlovid may need other medications adjusted, according to the agency.
The other antiviral pill option, molnupiravir, “has very few side effects, but you can't take it if you're pregnant,” the state agency said.
Doctors may also be reluctant to prescribe Paxlovid to younger adults, “not because it causes harm, but because in some studies it doesn't show as much benefit,” Chin-Hong said. In general, younger, healthier people are unlikely to die from COVID or become sick enough to require hospitalization, even without antiviral treatment.
But some data suggests that patients taking Paxlovid clear the coronavirus from their bodies more quickly.
“What we're finding is that people become negative very quickly on Paxlovid,” Chin-Hong said.
And a report, published in the journal Emerging Infectious Diseases, suggests that widespread use of Paxlovid “would not only improve outcomes in treated patients but also… reduce the risks of onward transmission.”
So if an initial doctor rejects a prescription for Paxlovid and you think you qualify, what other options are there?
One possibility is to contact another healthcare provider who may be more knowledgeable about Paxlovid and other antiviral medications or more willing to prescribe them.
Los Angeles County residents can call the county's public health information line, (833) 540-0473, to discuss treatment options with a healthcare provider.
Californians who are uninsured or struggling to obtain COVID-19 medications can schedule a free telehealth appointment by calling (833) 686-5051 or visiting sesamecare.com/covidca. Medication costs may be subject to a co-pay, depending on your insurance.
A program funded by the National Institutes of Health, featured at test2treat.org, gives adults who test positive for COVID-19 or the flu access to free telehealth care and treatment.