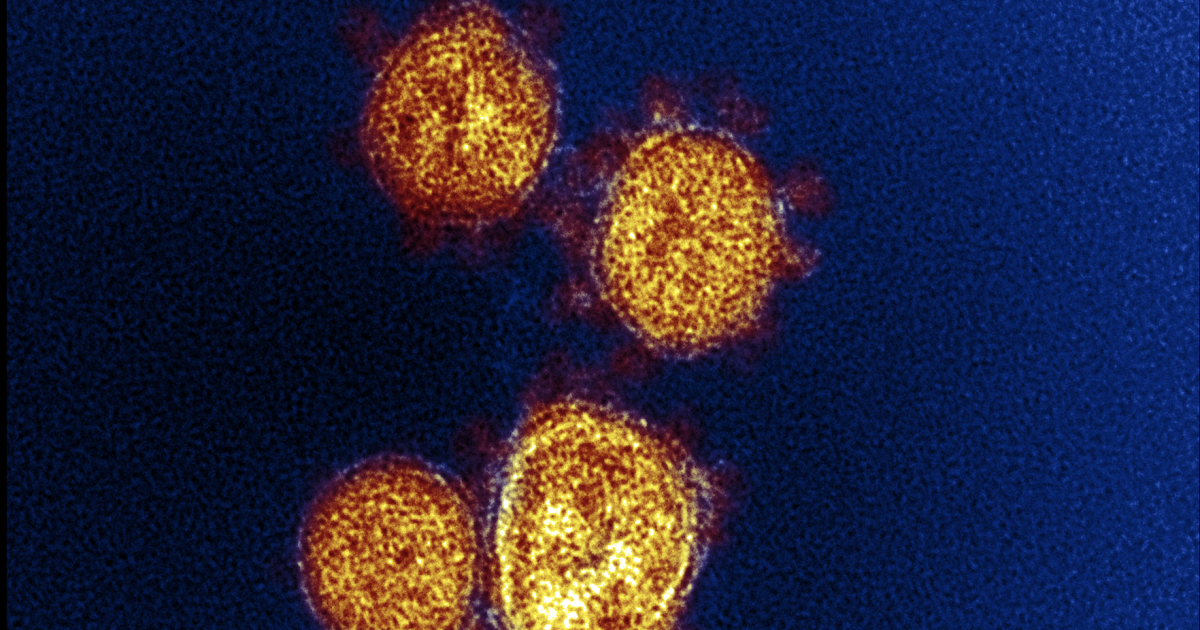
There are growing signs of a COVID-19 rebound in California thanks to the new FLiRT subvariants.
It is too early to know if FLiRT will make a major change to the COVID landscape and impacts have been small so far.
But health officials are taking note and urging Californians, especially those at risk, to be prepared.
Here's a summary of what we know and how you can protect yourself.
What are FLiRT subvariants?
The FLiRT subvariants, officially known as KP.2, KP.3 and KP.1.1, have overtaken the dominant winter variant, JN.1. During the two-week period ending Saturday, they were estimated to account for a combined 50.4% of the country's coronavirus infections, up from 20% the previous month.
Despite their greater transmissibility, the new mutations do not appear to cause more severe disease. And the vaccine is expected to continue working well, given that the new subvariants are only slightly different from the winter version.
“It's been quite a while since we've had a new dominant variant in the U.S.,” Dr. David Bronstein, an infectious disease specialist at Kaiser Permanente Southern California, told The Times earlier this month. “With each of these variants replacing the previous one, we see greater transmissibility: it is easier to transmit from person to person. So that’s really the concern with FLiRT.”
What are officials seeing?
Doctors say they are not seeing a dramatic increase in the number of seriously ill people and that COVID levels remain relatively low. But there are signs of a rise in infections that could cause the summer coronavirus season to start earlier than expected.
“COVID-19 concentrations in wastewater have suggested increases in several regions of California since early May. COVID-19 test positivity has been slowly increasing since May,” the state Department of Public Health said in a statement to the Times on Friday.
During the seven-day period ending Monday, about 3.8% of COVID-19 tests in California came back positive; at the end of April, that proportion was 1.9%. (Last summer's peak positive test rate was 12.8%, in late August.)
In San Francisco, infectious disease doctors are noticing more people in the hospital with pneumonia caused by COVID.
The Los Angeles County Department of Public Health has also begun to see a very small increase in cases in recent days. And Kaiser Permanente Southern California reports a small increase in outpatient COVID-19 cases.
How can I protect myself?
Vaccines
Doctors urged people to consider catching up on their vaccines, especially if they are at higher risk of serious complications from COVID-19.
In California, only 36% of people over 65 have received the updated COVID-19 vaccine that first became available in September. The U.S. Centers for Disease Control and Prevention has urged everyone over 6 months of age to receive a dose of the updated vaccine. A second dose is also recommended for people 65 years and older, as long as at least four months have passed since the last injection.
It is especially important that older people receive at least one updated dose. Of the patients he has seen recently who had severe COVID, said Dr. Peter Chin-Hong, an infectious disease specialist at UC San Francisco, all had not received an updated vaccine since September and were older or immunocompromised.
Behavior
Avoid sick people. Some sick people may pass off their symptoms as a “cold,” when it could be the beginning of COVID-19 illness.
Evidence
Test if you are sick and do it daily. Sometimes after the onset of illness, a rapid COVID-19 test takes longer to come back positive. Consider performing a rapid COVID test once a day for three to five consecutive days after the onset of cough and cold symptoms, said Dr. Elizabeth Hudson, regional chief of infectious diseases for Kaiser Permanente in Southern California. Doing so can help the sick person take steps to later isolate themselves and limit the spread of the illness to others.
Planning
Have a plan to order Paxlovid if you get sick. Paxlovid is an antiviral medication that, when taken by people at risk for severe COVID-19 who have mild to moderate illness, reduces the risk of hospitalization and death.
Masks are much less common today, but they can still be a useful tool in preventing infection. Wearing a mask on a crowded flight where people are coughing nearby can help reduce the risk of infection.
How can I protect my family and friends?
The US Centers for Disease Control and Prevention has recently eased COVID isolation guidelines, as the health impacts of COVID-19 are lower than before, due to the availability of vaccines, anti-inflammatory drugs, -COVID like Paxlovid and increased population immunity.
There are fewer people hospitalized and dying, and fewer reports of complications such as multi-inflammatory syndrome in children.
Still, doctors say it remains prudent to take common-sense steps to avoid getting sick and spreading the disease to others, given that COVID still causes significant health burdens that remain worse than the flu. Nationally, since early October, more than 43,000 people have died from COVID; By contrast, the flu has caused about 25,000 deaths during the same period.
While the prevalence of long COVID has been decreasing, long COVID can still be a risk whenever someone contracts COVID.
Here is a guide on what to do if you contract COVID-19:
Stay home and away from others while you are sick, plus one day after you recover
The CDC says people should stay home and away from other people in their household until at least 24 hours after their respiratory viral symptoms generally improve and they have had no fever (and are not using fever-reducing medications). Previously, the CDC suggested that people with COVID isolate for at least five days and take extra precautions for a few more days.
In terms of deciding when symptoms improve overall, what's most important is “the overall sense of feeling better and the ability to resume activities,” the CDC says. A persistent cough alone can last beyond someone being contagious, the CDC said.
The Los Angeles County Department of Public Health also recommends getting tested using a rapid test and getting a negative result before leaving isolation.
The agency also suggests staying away from the elderly and immunocompromised people for 10 days after you start feeling sick.
Take extra precautions after recovering in case you are still contagious
People who have recovered from COVID-19 may still be contagious for a few days after recovering. The CDC suggests taking extra precautions for five days after leaving your home and returning to spending time with others to keep others safe. They include:
- Wear a well-fitting mask;
- Continuing with COVID-19 testing. If it's positive, you're probably even more likely to infect others;
- Keep distance from other people;
- Increase air circulation by opening windows, turning on air purifiers, gathering outdoors if gathering with people;
- And continue with improved hygiene: wash and sanitize your hands frequently, clean high-touch surfaces, and cover coughs and sneezes.
Wear a mask for 10 days to protect others
The Los Angeles County Department of Public Health says people with COVID-19 should wear a well-fitting mask for 10 days after they start feeling sick, even if signs of illness are improving, to reduce the chance of other people becoming infected. Masks can be removed sooner if you have two consecutive negative results at least one day apart, the agency says.
Watch for COVID rebound
COVID rebound can occur when people with COVID-19 feel better, but then start to feel unwell two to eight days after they have recovered. Some people may also test positive again. COVID rebound may make you infectious again, capable of infecting those you interact with.
Rebound can occur whether you take Paxlovid or not.
Officials say if you feel sick again after recovering from COVID, again follow the same instructions of staying home and away from other people during the first phase of the illness.
If your test is positive but you have no symptoms
The CDC says if you never had any symptoms but tested positive, take extra precautions over the next five days, such as wearing a mask, getting tested, increasing air circulation, keeping your distance, and washing your hands frequently.
The Los Angeles County Department of Public Health recommends wearing a well-fitting mask for 10 days after testing positive for COVID-19, and also avoiding contact with high-risk people for 10 days after you start feeling sick, such as the elderly and immunocompromised. people. You can remove your mask sooner if you have two consecutive negative tests at least one day apart.
Los Angeles County health officials recommend that close contacts of people who have COVID-19 wear a well-fitting mask when around other people for 10 days after their last exposure. They suggest getting tested three to five days after your last exposure.