Unlike recent temperatures, California's COVID summer may no longer be heating up, though officials warn that the virus continues to circulate at high enough levels to have a potent infectious effect.
Still, any perceptible slowdown would be welcome news for the virus-weary state. And while it will take a few more weeks of measurements to confirm the trajectory, health officials hope the rollout of updated vaccines will help stem the tide even further.
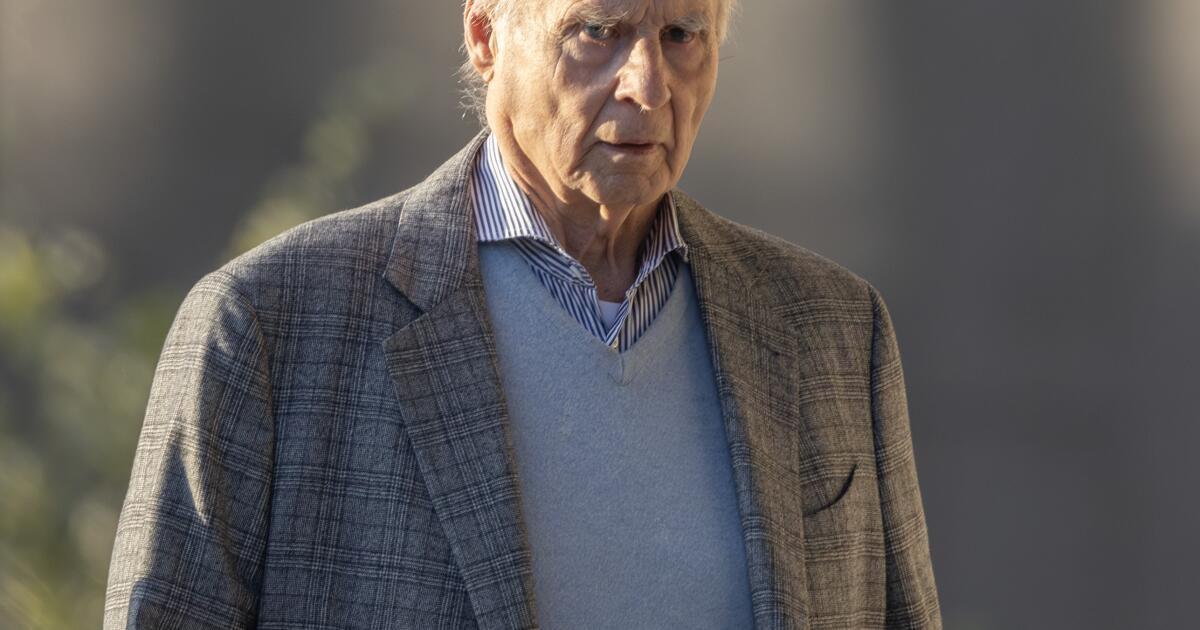
“It hasn't gone away, it's just decreased. It's just gone from 'very high' to 'high,'” said Dr. Peter Chin-Hong, an infectious disease expert at the University of California, San Francisco.
California has endured “high” levels of coronavirus in its wastewater since early June, and “very high” levels since July. But by the week ending Aug. 31 — the most recent data available — coronavirus levels in California’s wastewater had fallen back to “high,” according to the U.S. Centers for Disease Control and Prevention.
California is also now one of 16 states where COVID is estimated to be “declining” or “likely declining,” the agency said.
COVID levels in wastewater are considered “high” or “very high” in 44 states and the District of Columbia, and “moderate” in four. There were no estimates for the remaining two states, according to the CDC.
Other states where COVID is estimated to be “declining” or “likely declining,” according to the CDC, include Texas, Florida, New York and Illinois. COVID is thought to be “growing” or “likely growing” in seven states, including Michigan and Washington. COVID’s trajectory was “stable or uncertain” in 24 states and the District of Columbia, and there were no estimates for three states.
But not all metrics are pointing in the right direction, and doctors have warned that transmission could spike again due to travel and gatherings over the Labor Day weekend. It will take another week or more to get a better idea of how the holiday may influence COVID trends.
In California, more than 13% of coronavirus tests for which there is an officially recorded result came back positive during the week ending Sept. 2, higher than peaks seen both last winter and summer. A month ago, the figure was 12%, according to the California Department of Public Health.
In Los Angeles County, coronavirus levels in wastewater reached 75% of last winter’s peak during the 10-day period ending Aug. 24. That’s down from the 86% reading for the 10-day period ending Aug. 17.
Official coronavirus case counts have been declining, though reporting may have been halted by the Labor Day holiday.
During the week ending Sept. 1, an average of 381 coronavirus cases were reported per day in Los Angeles County, down from 410 the week before. Those counts include only confirmed infections in medical institutions and do not reflect results from at-home testing. Fewer people are getting tested when they are sick.
“I would say we’re seeing some sort of surge in cases,” said Dr. Elizabeth Hudson, regional chief of infectious diseases for Kaiser Permanente Southern California.
There are certainly new COVID patients coming into doctors' offices and clinics, but overall numbers through Friday no longer appear to be accelerating like they were a month ago, Hudson said.
The percentage of coronavirus-related emergency room visits in Los Angeles County has remained at a relatively high level for the past six weeks, between 3.7% and 4.3%. It peaked at 5.1% last summer.
Coronavirus-related hospitalizations in Los Angeles County remain relatively high for this summer, but they are not increasing. During the week ending Aug. 31, there were an average of 447 coronavirus-positive people in Los Angeles County hospitals per day, down from the previous week’s seasonal high of 499. Last summer’s peak was 620.
In the San Francisco Bay Area, coronavirus levels in wastewater have also declined. Coronavirus levels are now considered “medium” in sewers in San Jose and Palo Alto, and “low” in Sunnyvale, according to the Santa Clara County Public Health Department.
And at University of California, San Francisco hospitals, there were about 10 coronavirus patients as of Friday, down from the seasonal peak of about 30.
COVID-19 deaths have been rising, an expected development that reflects increased transmission over the summer. Los Angeles County averaged about 2.7 COVID-19 deaths per day during the week ending Aug. 13, the most recent for which data is available, down from an average of between 1 and 2 that had held steady since early July.
Deaths have also been rising nationally. In the week ending Aug. 10, 971 COVID deaths were reported. That’s more than double the weekly count since early summer, but only two-thirds of the peak numbers from mid-year 2023.
In a statement, the Los Angeles County Department of Public Health said it “will continue to monitor COVID-19 data in the coming weeks to better understand whether we are truly past this summer’s peak.”
While COVID-19 may be on the decline for now, doctors are urging people to get vaccinated against COVID-19 and the flu in the fall, when both viruses typically start to gain strength. Australia recently suffered a major wave of flu during the winter, and American doctors see the country’s experience as a possible sign of things to come.
“Flu season started early with a high number of cases… We expect the flu season to be quite intense,” Hudson said. “Getting a flu vaccine now ensures protection throughout the flu season.”
The CDC recommends that everyone 6 months or older get the updated COVID-19 and flu vaccines this season. The best months to get them are September and October, according to the CDC, and people can get both doses at the same visit.
There are also ways to get a flu shot without getting a shot. One option, called FluMist, is available as a nasal spray for non-pregnant people ages 2 to 49. Another needle-free flu vaccine option is called Afluria.
As for exactly when the ideal time to get vaccinated is, doctors offered mixed advice.
Hudson suggested getting both vaccines now, as she has already done.
“It’s so easy for all of us to … procrastinate,” she said. “Now is the time to really do it. Do it before we start dealing with everything that comes with the holidays, with the kids going back to school.”
Vaccines have been widely available at stores including CVS, Walgreens, Rite Aid, Ralphs, Vons, Albertsons, Pavilions and Safeway. Starting Monday, updated COVID vaccines will be available at Kaiser locations in California for people ages 5 and older. For infants and younger children, vaccines will likely be available by mid-September.
Sutter Health expects to begin offering COVID vaccines in mid- to late September.
“Taking one of these vaccines is a very good way to potentially stop this current wave in its tracks,” Hudson said.
Chin-Hong suggested it's important for older and immunocompromised people to get vaccinated now if they haven't gotten a COVID shot in a year or more. But for younger people who aren't immunocompromised, she suggested the ideal time to get a COVID and flu vaccine is October, which would be closer to the expected peaks of the fall and winter COVID and flu season.
Older people who were last vaccinated in the spring can likely wait until October to get another dose, Chin-Hong said.
The COVID-19 vaccine will boost protection against severe disease and hospitalization for at least a year, Chin-Hong said. But one reason to consider waiting until October is that the best protection against infection comes about six to eight weeks after getting the vaccine. That window may be wider if the vaccine is a close match to circulating subvariants, Chin-Hong said.
He said he plans to get his COVID and flu vaccines in mid-October.
If you're trying to time your COVID vaccination to get maximum protection from infection before a major event, such as a vacation, about two weeks out is a safe bet. Chin-Hong said immunity kicks in just a few days after the shot, but the greatest benefit is achieved about a week or two later.
It is also especially important for expectant mothers to get vaccinated against COVID.
“If they want to protect the baby, they should get the vaccine at least two weeks before delivery,” Chin-Hong said. “The antibodies have to cross the placenta,” and that takes time.
Wearing masks in indoor public spaces also remains a prudent idea for those looking to avoid getting infected, Hudson said.
Reducing your risk of contracting COVID-19 also reduces your risk of long COVID-19 and the significant health problems it can cause. Sérgio Mendes, the legendary Grammy-winning Brazilian musician, died Thursday at age 83 in Los Angeles, with his family saying his health “had been affected by the effects of long COVID-19.”
Generally speaking, long COVID can contribute to a wide variety of ailments, including difficulty breathing and shortness of breath, as well as difficulty maintaining blood pressure. In some people, long COVID can trigger a range of health problems that persist for months or even years.
CDC also recommends respiratory syncytial virus (RSV) vaccination for everyone 75 years and older, as well as for adults 60 to 74 years at higher risk for severe RSV. The RSV vaccine is not annual, meaning people who received one last year do not need to get another one at this time, the CDC said. It can also be given during the same visit as the flu and COVID vaccines.
There is also an RSV vaccine for pregnant women between 32 and 36 weeks of pregnancy to provide protection to their fetuses. There is also an RSV antibody for infants and some young children.
Times staff writers August Brown and Alexandra Del Rosario contributed to this report.