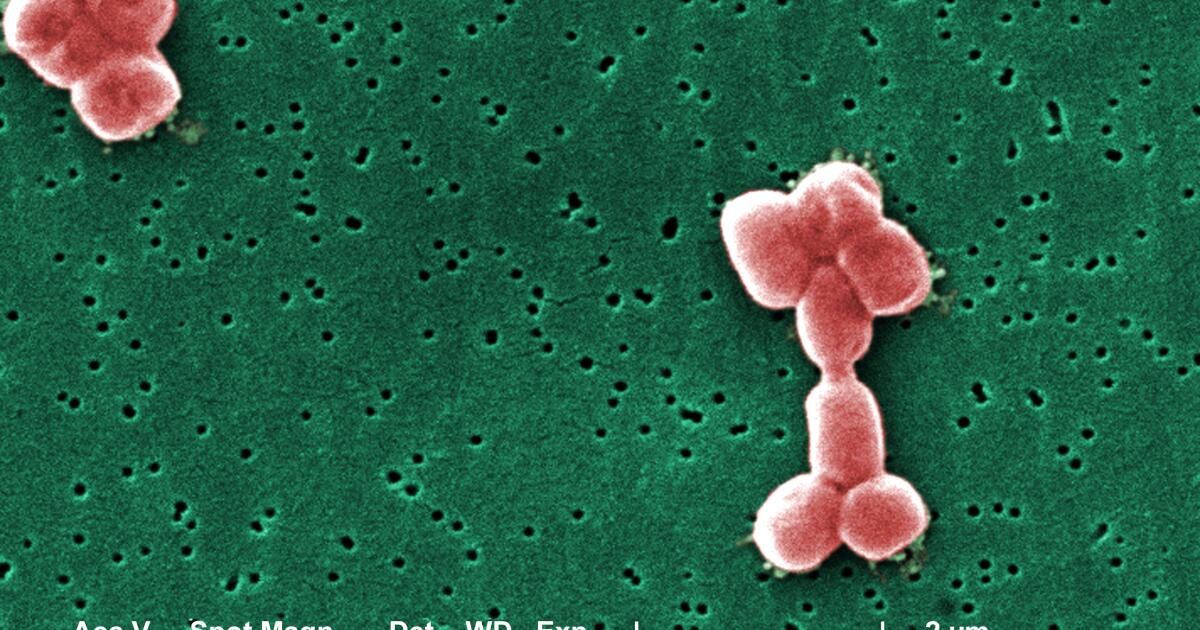
Under the microscope, this drug-resistant superbug appears as benign as a handful of rocks. However, resistant to carbapenems Acinetobacter baumanniior CRAB, is a nightmare for hospitals around the world, killing approximately half of all patients who acquire it.
Identified as a top priority pathogen by both the World Health Organization and the US Centers for Disease Control and Prevention, CRAB is the most common form of a group of bacteria that are resistant to almost all available antibiotics. The victims are usually hospitalized patients who are already sick with blood infections or pneumonia. In United States alonethe virus sickens thousands and kills hundreds each year.
But 2024 begins with some encouraging news on the global health front: For the first time in half a century, researchers have identified a new antibiotic that appears to effectively kill A. baumannii.
The compound, zosurabalpin, attacks bacteria from a novel angle, altering the route that a key toxin follows on its journey from the inside of the bacterial cell to the outer membrane that protects the insect from the immune system’s defensive attacks.
No other antibiotic approved by the U.S. Food and Drug Administration takes this approach, and the element of surprise is a major advantage even against microscopic enemies. A. baumannii has had no chance to develop resistance against the drug, meaning that, at least for a time, zosurabalpin could prevent serious illness and death.
“As far as I can tell, the scientific approach is brilliant,” said Dr. Oladele A. Ogunseitan, a professor of population health and disease prevention at UC Irvine, who was not involved in the study.
The drug was jointly developed by scientists from the Swiss pharmaceutical company Roche and Harvard University. His recommendations They were published Wednesday in the journal Nature.
Carbapenem resistant A. baumannii is a type of Gram-negative bacteria, a puzzling category of superbugs. Encased in an inner and outer membrane that antibiotics struggle to cross, Gram-negative bacteria are resistant to most currently available therapies. They are also surprisingly cunning for single-celled organisms, with the ability to quickly develop new defenses against antibiotics and then pass them on to other bacteria through genetic material.
Antibiotic-resistant superbugs claim the lives of more than 1 million people worldwide each year. The rise of drug resistance is partly due to human folly (we have long overprescribed and abused antibiotics), but it is also because bacteria continually find ways to evade threats. Over the past 50 years, these pathogens have developed defenses faster than we can produce new drugs.
In their search for a new weapon, scientists at Roche and Harvard turned their attention to a group of compounds called linked macrocyclic peptides. After testing a library of 45,000 MCPs, the researchers found one that seemed especially lethal against A. baumannii. After some chemical tinkering, that compound became zosurabalpin.
“This is a very promising development,” said Paul J. Hergenrother, a chemistry professor at the University of Illinois who was not involved in the research but wrote about the findings for Nature. “Zosurabalpin kills bacteria in a different way than all other approved antibiotics.”
The drug takes action only in the presence of lipopolysaccharide, a bacterial toxin. LPS is produced within the bacterial cell and transported by a unique transport system to the insect’s external defenses.
“The bacterial outer membrane is important for bacteria because it helps them live in difficult conditions and survive attacks by our immune system,” said Kenneth Bradley, global head of infectious disease discovery at Roche.
Zosurabalpin essentially cuts off the LPS transport route. Without a way to reach the cell’s outer membrane, where it can begin to fight off drug and immune attacks, the toxin builds up inside the bacteria and eventually kills the cell.
In mouse studies, the drug effectively eliminated CRAB infections in the blood, lungs and thighs, a selection that mirrors the way the insect infects humans.
It is currently in Phase I trials in humans, where researchers are looking at safety, tolerability and how much of the chemical remains in patients’ bodies over time, said Michael Lobritz, head of infectious diseases at Roche. .
“It has been more than 50 years since the last distinct class of antibiotic capable of treating gram-negative bacterial infections was released,” Lobritz said in an email. “Any new class of antibiotic that has the ability to treat infections caused by multidrug-resistant (MDR) bacteria, such as those resistant to carbapenems Acinetobacter baumannii (CRAB) would be a significant advance.”
As encouraging as the early results are, scientists stressed that it would be foolish to become arrogant in the fight against a virus that, time and time again, has found ways to evade our most advanced pharmaceutical weaponry.
“Resistance has emerged to every antibiotic ever created, and resistance to zosurabalpine is also likely to emerge in the future, if it is successfully developed into a clinical antibiotic,” Bradley said.
In their findings, the authors noted some genetic mutations in the laboratory that significantly reduced the drug’s success against A. baumannii. These were rare but worrying; a rare mutation reduced the drug’s effectiveness 256 times.
“Although the rates of emergence of these resistant organisms are low and comparable to those of standard antibiotics, the observation affirms the principle that we can never rest on our laurels with the chemical and biochemical warfare we are waging against bacterial pathogens. “Ogunseitan said.
Zosurabalpin is essentially unknown to bacteria. If it is safe and effective in humans, there is likely to be a limited period in which it can effectively save lives and prevent suffering. But no matter how sophisticated our tools are, the scientists said, these potentially deadly cells will always have a big advantage against us.
“Bacteria have a huge numerical advantage: there can be billions of them in a flask,” Hergenrother said. “Bacteria will eventually develop resistance to virtually all antibiotics, which is why we need a constant supply of new antibiotic candidates.”