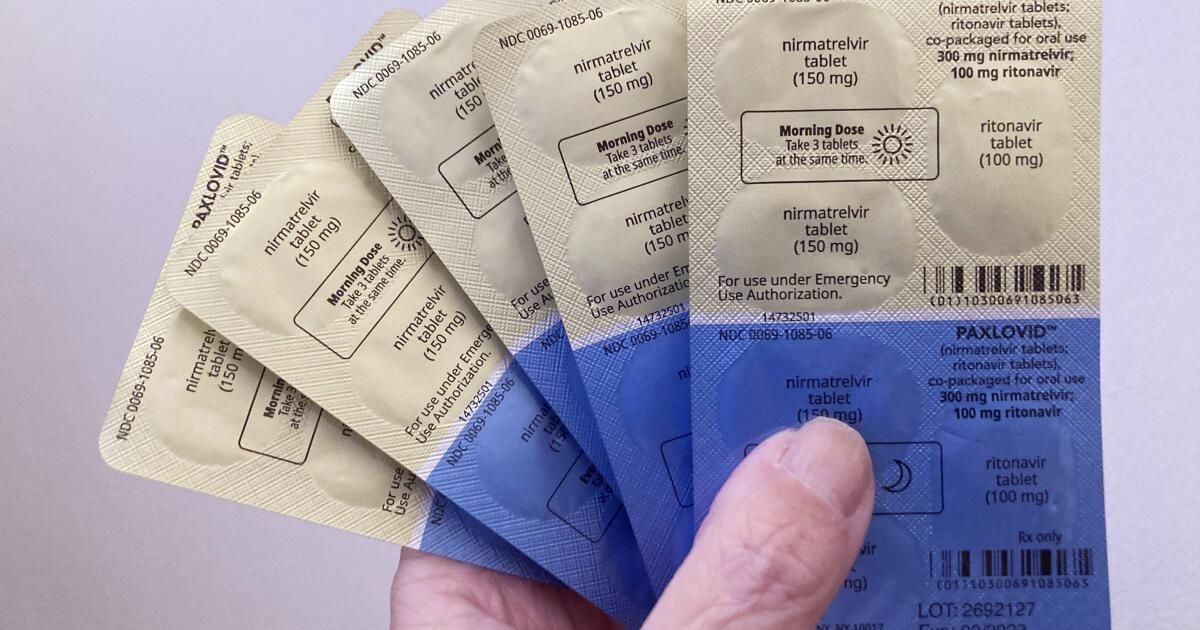
To the editor: The timing of your article about doctors' reluctance to prescribe the antiviral drug Paxlovid to COVID-19 patients is perfect.
The test for the disease came back positive on January 31. I called my doctor and they recommended that I not take Paxlovid unless I felt worse. The reason? COVID rebound.
But the Paxlovid order was placed at my Vons pharmacy. Guess what? They don't carry it and haven't for months. The order was then sent to CVS. They had it.
My wife went to pick him up. Guess what? They wanted $1,100.
I have Medicare with a Blue Shield supplement, so you can imagine our surprise at the price. Needless to say, I did not receive the medication.
It's fascinating to read this article saying that the COVID rebound is a myth and that Paxlovid is free or very cheap for most people. But in my experience, drugs are not free. Paxlovid may work, but I'll be damned if I pay $1,100 for it.
Mike Moersen, Thousand Oaks
..
To the editor: I tested positive for COVID last week. My doctor prescribed Paxlovid. Masked, I went to CVS and was told my insurance did not cover Paxlovid.
I asked how much Paxlovid costs and they said $1,000. My insurance is Blue Cross of California and Medicare Parts A and B.
Margarete O'Brien, Manhattan Beach
..
To the editor: My husband and I traveled this year and our doctor prescribed Paxlovid for us to take with us in case we contracted COVID while we were away. We also did this last year and never had to use the drug.
Last year, our copay was $5 each. This year Medicare will not cover the drug, so it would cost us $1,000 each.
I find it inexcusable that Medicare and Aetna, our private insurer, do not cover my 80-year-old husband and me, 77, for Paxlovid. Being hospitalized with COVID would far exceed the cost of being treated with Paxlovid. Has no sense.
Janine Lichstein, Santa Monica