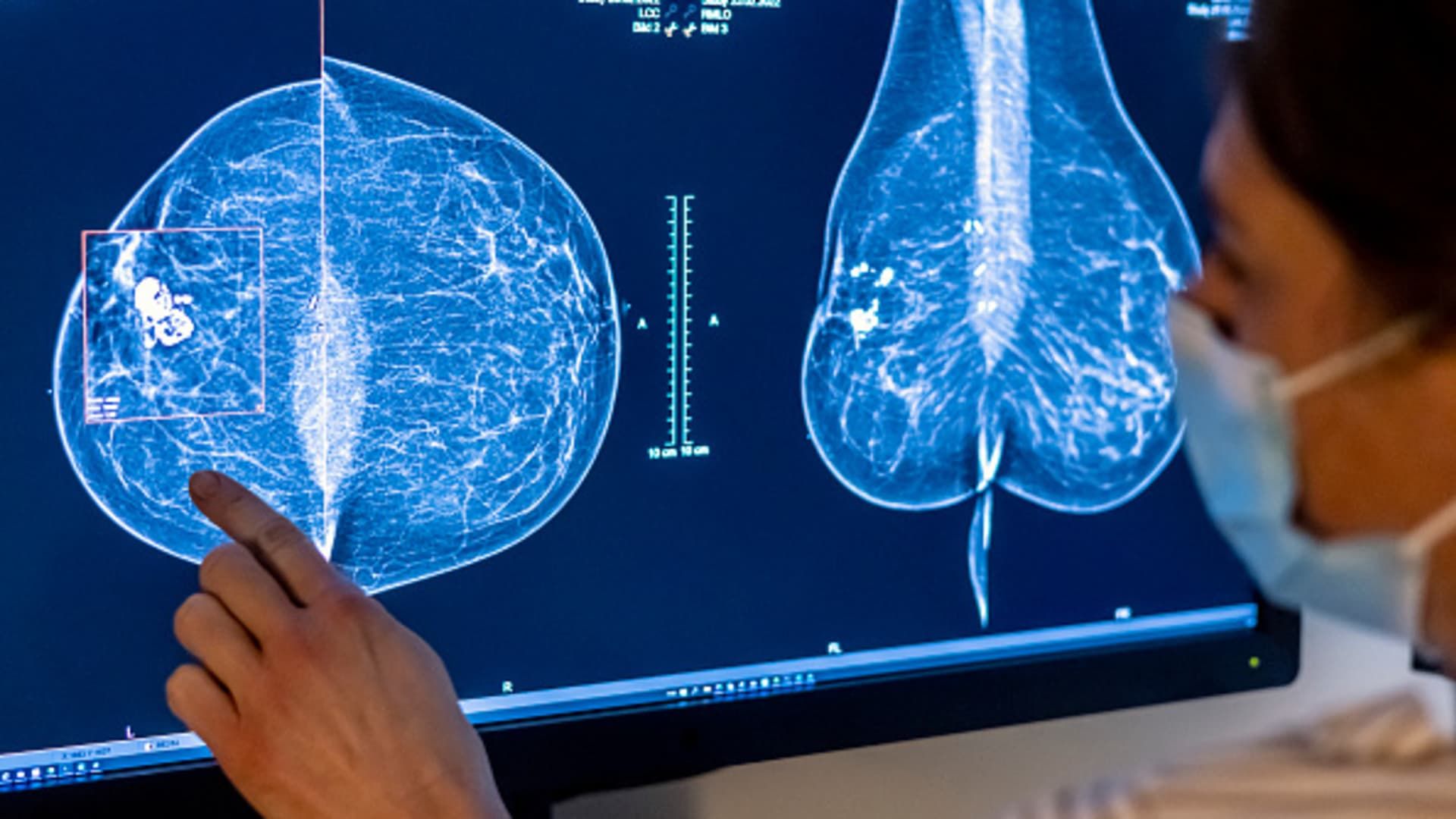
Medical personnel use a mammogram to examine a woman's breast for breast cancer.
Hannibal Hanschke | dpa | Image Alliance | fake images
Cancer drains people of their physical, emotional and financial health. Given the impact on both patients and the people around them (including their employer), it is time for CEOs to take note and take action to reduce the burden of cancer.
In a study by the American Cancer Society's Cancer Action Network, nearly half of cancer patients and survivors reported being unusually burdened by medical debt. Many respondents had a negative balance of at least $5,000 from their cancer treatment for more than a year, and 42% of people with cancer exhaust their life savings within the first two years after diagnosis.
Financial hardship caused by cancer can also contribute to “financial toxicity,” in which the cost of treatment forces individuals to make trade-offs that affect their chances of survival. These may include nonbiological factors, such as skipping or halving cancer medications to stretch your supply, or not being able to complete cancer care as planned due to high transportation or lodging costs near treatment centers. of cancer. This model is not sustainable, and the rising costs of new, life-saving cancer therapies will impose additional financial toxicities and an increasing threat to patients' lives.
The financial toxicity of cancer care not only affects the individual, but can also negatively affect their employer. As providers of health insurance coverage for nearly half of the country, employers and unions bear much of the financial burden of cancer. Today, cancer is the leading healthcare cost for mid-sized and large organizations in the U.S., and the burden is growing.
For the first time in history, more than 2 million Americans will receive a new cancer diagnosis in 2024. While the increase in cancer incidence can be attributed in part to our aging population (cancer risk increases with age) , we also see a worrying national trend in which younger people are being diagnosed with 17 major types of cancer. These are people who would likely still be in the workforce and using employer-sponsored health insurance. As a result, employers are asking what they can do to reduce the burden of cancer on their populations and their bottom lines.
Patients, families, and employers “win” when cancers are diagnosed at an early stage. Early detection of cancer not only improves the chances of survival, but also significantly reduces the cost of care. Overall, treatment costs for someone diagnosed at stage IV (when the cancer has spread throughout the body) are an average of $156,000 higher than those diagnosed at stage I, when the disease is localized. The first year of treatment for colorectal cancer, which affects more than 150,000 people each year in the United States and is increasing in younger populations, costs an average of $111,000 when diagnosed at stage I, with a survival rate five years of approximately 90%. . In contrast, stage IV colorectal cancer results in average treatment costs of $256,000 in the first year, and five-year survival rates are less than 20%. Evidence suggests that if people could take advantage of the cancer prevention, early detection, and treatment strategies that exist today, the cancer mortality rate would decrease by 30% to 50%.
These statistics are profound and strongly suggest that concerted efforts by employers and individuals to encourage cancer prevention and early detection would improve health and reduce health care costs. Today, our best tool to achieve this is screening. Adherence to recommended screening guidelines, such as those published by the ACS, could save the US healthcare system $26 billion a year in avoided treatment costs.
Despite the importance of early detection and the proven value of screening, access to preventive care remains a barrier to better outcomes. Currently, a staggering 65% of eligible Americans are not up to date with recommended cancer screenings. Covid-19 restrictions delayed or prevented 9.4 million cancer screenings in 2020 alone, likely leading to later-stage diagnoses that would normally have been detected earlier.
There are also logistical and social barriers that contribute to financial toxicity and impact a person's ability to get screened. People may need to take time off work or arrange childcare to attend a screening appointment. They may have to weigh the possible future costs of treatment against their need to pay rent. Some people may not know they are eligible for screening, and the stigma and fear associated with cancer screening prevents some people from seeking care. Inequalities based on a person's socioeconomic status (including where they live, their income, their educational level, access to health care and healthy foods, and other social determinants of health) create barriers to preventive care. To reap the benefits of early detection in individuals and organizations, it is important that we develop new strategies to eliminate these barriers.
Karen Knudsen, CEO of the American Cancer Society
NYSE
ACS is committed to the fight against cancer, addressing the challenge of improving access to care and reducing financial toxicity from multiple angles. Similar or supportive action by American employers will increase our collective impact against the burden of cancer.
With the goal of increasing early detection, ACS recently partnered with Color Health in a joint venture to improve access to screening and preventive care through employers and unions. By making it easier and more convenient for employees to receive care (with at-home testing kits and support for navigating care throughout their cancer journey), this program aims to increase awareness, accessibility and affordability of cancer screening and early detection tests. In particular, organizations leveraging the ACS-Color program have witnessed a 77% increase in cancer screening compliance.
In addition to direct screening initiatives, programs such as Road to Recovery and ACS Hope Lodges eliminate transportation and lodging costs for cancer treatment. Other partnerships through BrightEdge, the donor-funded investment and innovation arm of ACS, provide access to a broad range of solutions that help people navigate the financial complexities of cancer across the continuum of care. A BrightEdge portfolio company, TailorMed, offers a platform to help patients find resources to cover the cost of treatment and reduce out-of-pocket expenses. Other investments aim to bring the patient voice to the development of therapies and diagnostics, to enable a future generation of sustainable cancer innovations that reduce financial hardship for patients.
Promotion is also key to reducing financial toxicity. The ACS Cancer Action Network advocates for Medicaid expansion to help people who are currently uninsured access screenings and preventive care. To reduce the cost of prescription drugs, ACS CAN has also successfully advocated for a “smoothing” policy, which allows Medicare beneficiaries to spread the costs of their prescription drugs throughout the year. By making payments more manageable for patients, we eliminate a crucial element of the financial challenge of cancer.
Cancer will affect one in two women and one in three men at some point in their lives. By facilitating guideline-recommended screening and activating programs that make early detection affordable and accessible, employers can offset financial toxicities and improve outcomes for people across the country. When employers help their employees get screened, they bring us one step closer to ending cancer (and its costs) as we know it.
—By Karen Knudsen, CEO of the American Cancer Society (ACS) and the American Cancer Society Cancer Action Network (ACS CAN). She is also a member of the CNBC CEO Council.