In a photo illustration, prescription medications are seen next to a bottle of pills on July 23, 2024 in New York.
Spencer Platt | Getty Images News | fake images
A coalition of patient advocacy groups is urging a federal court to stop the practices of third-party companies that purchase drugs from countries outside the FDA-regulated U.S. supply chain, which the groups say put the health of American patients at risk.
The court filing comes in the wake of a CNBC investigation that documented how these third parties, commonly known as alternative financing programs or AFPs, have spread to employer-sponsored health plans across the country. Under the growing business model, AFPs source high-cost specialty drugs from abroad at lower prices and charge employers a fee or a percentage of the savings. The AFPs then provide the medications to patients at little or no cost.
AFPs are especially attractive to small employers, such as local school districts, county governments and others that pay out-of-pocket for their staff's health care costs. But there's a trade-off: Federal officials from the U.S. Department of Homeland Security and the Food and Drug Administration told CNBC that these drugs are being imported illegally and putting patients' lives at risk. Last year, a Homeland Security Investigations official told CNBC that criminal investigations were underway into the AFP.
The filing before a U.S. Court of Appeals in Maryland, dated December 26, was led by the HIV+Hepatitis Policy Institute, a nonprofit organization that advocates for safe and affordable treatment for people living with HIV and viral hepatitis.
“Forcing a person who has employer-sponsored health insurance to enroll with an unknown third-party provider to receive their lifesaving medication supplied by a foreign country is not only illegal but endangers the health and safety of patients,” wrote Carl Schmid, executive director of the HIV+Hepatitis Policy Institute, in a news release. “While federal regulators should shut them down, in the meantime, courts must step in to protect patients.”
In the court filing, patient groups said the agreements can delay treatment, confuse patients and expose them to drugs that differ from those distributed through the tightly regulated U.S. system. They warned that patients with chronic and life-threatening illnesses should not be forced to trade the safety and certainty of approved U.S. supply chains for lower costs to employers.
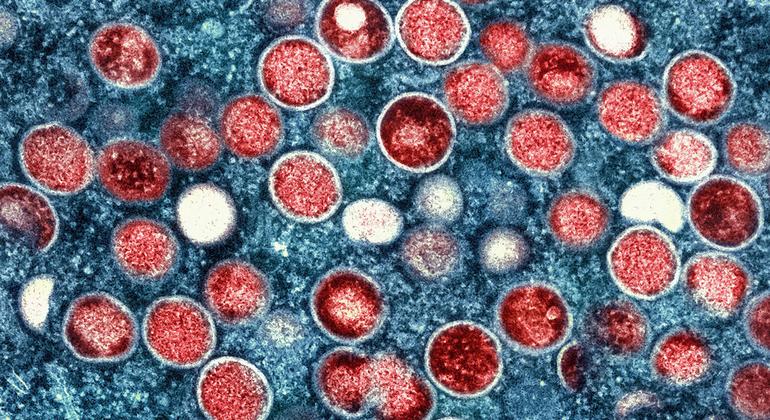
The amicus curiae brief was filed in a case brought by Gilead Sciences after the company learned that an HIV patient received a Gilead drug with a label written in Turkish. Gilead alleges that the drug traveled through an unsecured supply chain that does not comply with US law. Türkiye is a known hotbed of counterfeit drugs, according to U.S. officials.
Gilead sued several companies involved in administering employer health plans, including the Rx Valet alternative financing program.
Greg Santulli, CEO of Georgia-based AFP, told CNBC last year that he is confident in the safety of the drugs his company sources, adding that Turkey is a “modern and sophisticated country” capable of tracking drugs through its supply chain.
The lawsuit also names Meritain Health, which administered the patient's employee health plan and is owned by CVS Health.
A CVS Health spokesperson told CNBC last year that it “has long maintained a policy of not supporting programs for non-FDA approved drugs from outside the United States and not contracting with companies to facilitate the importation of non-FDA approved drugs” from abroad.
A federal judge issued a preliminary injunction preventing all parties in the case from importing Gilead drugs from abroad. The defendants are appealing the ruling and Meritain argues that the court order is unnecessary and would negatively affect its business. Rx Valet in a court filing said the court order undermines access to safe medications, adding that Gilead's HIV drug shipped from Turkey was the same one sold in the U.S. at a much higher cost.