But what is it, where does it come from, and how can the world confront the threat, which inevitably raises the spectre of past pandemics such as COVID-19 and the early spread of HIV infections?
Here's what you need to know:
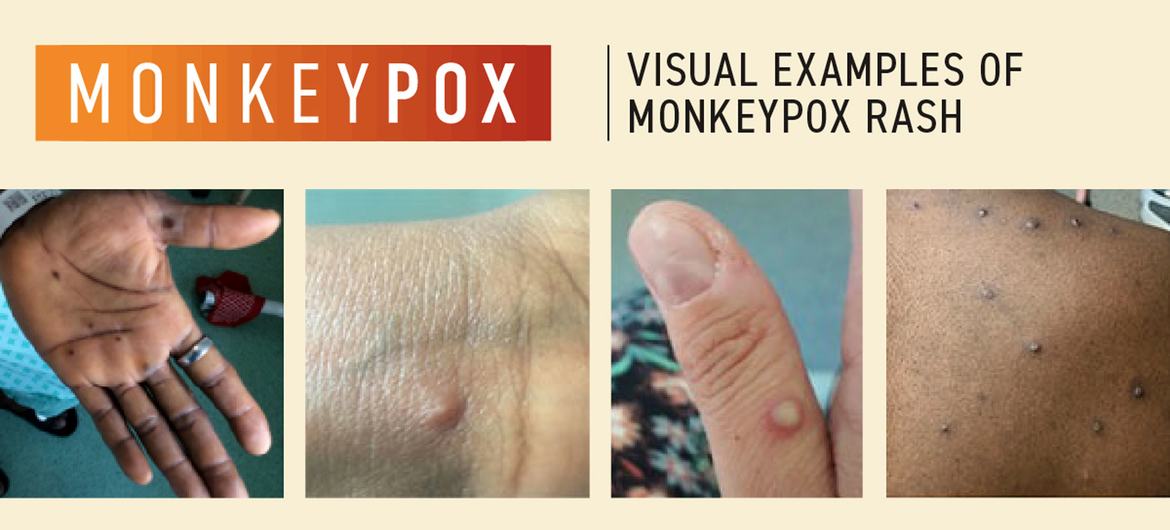
Mpox lesions usually appear on the palms of the hands. (file)
What is mpox?
Formerly known as monkeypox, the viral disease can spread between people, mainly through close contact, and occasionally from the environment to people via objects and surfaces that have been touched by a person with monkeypox.
Mpox, which originated in the Democratic Republic of Congo in the 1970s, has been neglected there, according to the WHO.
“It is time to act decisively to prevent history from repeating itself,” said Dimie Ogoina, who chairs the International Health Regulations Emergency Committee, which advises WHO on these issues.
The infectious disease, endemic in central and western Africa, subsequently caused a global outbreak in 2022, leading to a WHO public health emergency in July as it became a multi-country outbreak.
Following consultations with global experts, WHO has begun using a new preferred term, “mpox,” as a synonym for monkeypox. Learn more about that decision here.
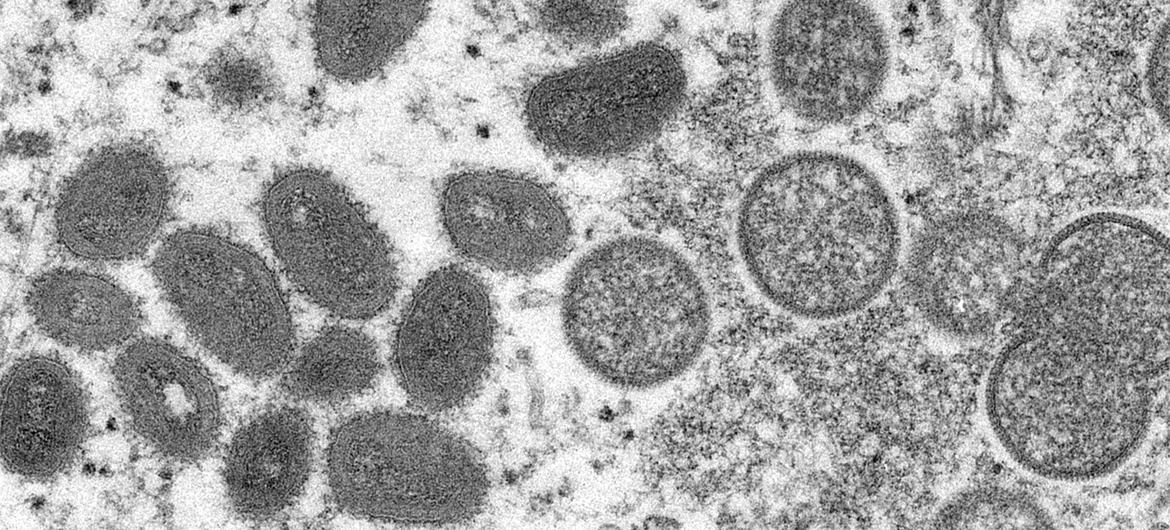
Mpox is similar to the eradicated smallpox virus. (file)
What are the symptoms?
Common symptoms of MPOX include a rash that lasts two to four weeks and may begin or be followed by fever, headache, muscle aches, back pain, lack of energy, and swollen lymph nodes.
The rash is blister-like and may affect the face, palms of the hands, soles of the feet, groin, genital and/or anal areas, mouth, throat, or eyes. The number of sores may vary from one to several thousand.
People with MPOX are considered contagious at least until all blisters have crusted over, the scabs have fallen off and a new layer of skin has formed underneath, and all lesions in the eyes and on the body have healed. This usually takes two to four weeks. Reports show that people can become reinfected after having MPOX.
People with severe MPOX may require hospitalization, supportive care, and antiviral medications to reduce the severity of the injury and shorten recovery time.
WHO continues to work with patients and community advocates to develop and disseminate information tailored to communities affected by monkeypox.
How does mpox spread?
From human to human: Touching, having sex with, talking to or breathing near someone with mpox can generate infectious respiratory particles, but more research is needed on how the virus spreads during outbreaks in different settings and conditions, WHO says.
What scientists do know is that the virus can also persist for some time on clothing, bedding, towels, objects, electronic devices and surfaces that have been touched by a person with mpox. Another person who comes into contact with these items can become infected without first washing their hands before touching their eyes, nose and mouth.
The virus can also be transmitted during pregnancy to the fetus, during or after birth through skin-to-skin contact, or from a parent with mpox to an infant or child during close contact.
Although there have been reports of people contracting MPOX from someone who is asymptomatic, there is still limited information about whether the virus can be transmitted from someone with the virus before they have symptoms or after their lesions have healed.
From humans to animals: Since many animal species are known to be susceptible to the virus, there is a possibility that the virus may be transmitted from humans to animals in different environments.
People with confirmed or suspected MPOX should avoid close physical contact with animals, including pets such as cats, dogs, hamsters, and gerbils, as well as livestock and wildlife.
From animals to humans: MPOX virus can also be contracted by someone who comes into physical contact with an animal that carries the virus, such as some species of monkeys or ground rodents such as squirrels. This exposure can occur through bites or scratches, or during activities such as hunting, skinning, trapping, or preparing a meal. The virus can also be contracted by eating contaminated meat that is not thoroughly cooked.

A health worker monitors a two-year-old boy receiving treatment for mpox north of Goma, Democratic Republic of Congo.
Can it be fatal?
Yes, for a small minority. Between 0.1 and 10 percent of people who have been infected with MPOX have died.
It is important to note that mortality rates in different settings may differ due to several factors, such as access to health care and underlying immunosuppression, including due to undiagnosed HIV or advanced HIV, according to the UN health agency.
In most cases, MPOX symptoms go away on their own within a few weeks with supportive care, such as medications for pain or fever, but in some people, the illness can be severe or lead to complications and eventually death.
Newborns, children, pregnant people, and people with underlying immune deficiencies (such as those caused by advanced HIV) may be at increased risk of more severe mpox disease and death.
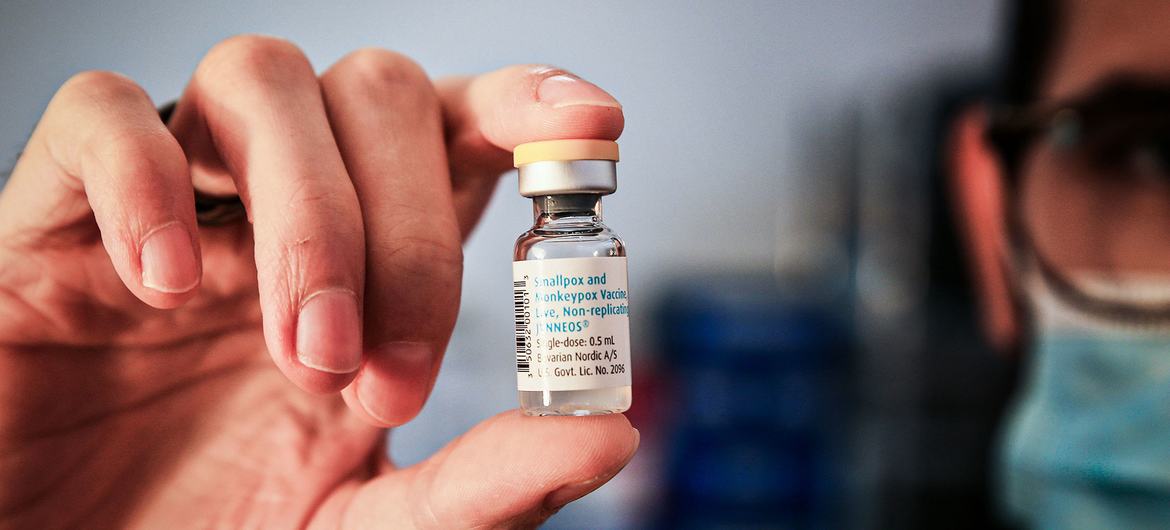
A single dose of the mpox vaccine.
Is there a vaccine?
Yes. The UN health agency recommends several vaccines against mpox. However, mass vaccination, which was implemented during the global COVID-19 pandemic, is not currently recommended.
Many years of research have led to the development of newer, safer vaccines against smallpox, a disease that has now been eradicated. Some of these vaccines have been approved in several countries for use against smallpox.
Currently, WHO recommends the use of the MVA-BN or LC16 vaccines, or the ACAM2000 vaccine when the others are not available.
According to WHO, only people who are at risk of exposure to mpox should be considered for vaccination. Travelers who may be at risk based on an individual risk assessment with their healthcare provider may wish to consider vaccination.

One way to prevent the spread of MPOX is to wash your hands after touching contaminated surfaces.
How can you prevent mpox?
Cleaning and disinfecting surfaces or objects and cleaning your hands after touching surfaces or objects that may be contaminated can help prevent transmission.
The risk of contracting MPox from animals can be reduced by avoiding unprotected contact with wild animals, especially those that are sick or dead, including their meat and blood.
In countries where animals carry the virus, any food containing animal parts or meat should be thoroughly cooked before consumption.
Learn more about mpox here.












