In an alert, the WHO noted that although only eight percent of hospitalized coronavirus patients also had bacterial infections that can be treated with antibiotics, a staggering three out of four received them “just in case.”
At no point during the global pandemic did the UN health agency recommend the use of antibiotics to treat COVID-19, insisted WHO spokesperson Dr. Margaret Harris.
Viral, not bacterial
“The advice was very clear from the beginning that this was a virus. “So it's not that there was any guidance or recommendation for doctors to go in this direction, but maybe because people were dealing with something completely new, they were looking for what they thought might be appropriate.”
According to the UN health agency, antibiotic use ranged from 33 percent in patients in the Western Pacific region to 83 percent in the Eastern Mediterranean and African regions. Between 2020 and 2022, prescriptions decreased over time in Europe and the Americas, but increased in Africa.
Last hope
Data collected by the WHO also indicated that the majority of antibiotics were given to critically ill COVID-19 patients, with a global average of 81 percent. Antibiotic use in mild or moderate infections showed considerable variation between regions, with the highest use in Africa, at 79 percent.
Worryingly, the UN agency found that the bacteria-destroying antibiotics most commonly prescribed around the world were those with the greatest potential for antimicrobial resistance (AMR).
“When a patient requires antibiotics, the benefits often outweigh the risks associated with side effects or antibiotic resistance. However, When they are unnecessary, they offer no benefit and pose risks.and its use contributes to the emergence and spread of antimicrobial resistance,” said Dr. Silvia Bertagnolio, head of WHO's surveillance, evidence and laboratory strengthening unit for antimicrobial resistance.
No positive impact
The UN health agency report stated that The use of antibiotics “did not improve the clinical outcomes of patients with COVID-19”.
Instead, its systematic prescription “could create harm for people without bacterial infection, compared to those who do not receive antibiotics,” the WHO said in a statement.
“These data call for improvements in the rational use of antibiotics to minimize unnecessary negative consequences for patients and populations.”
The findings were based on data from the WHO Global Clinical Platform for COVID-19, a database of anonymized clinical data from hospitalized coronavirus patients. The data comes from 450,000 patients in 65 countries from January 2020 to March 2023.
Superbacteria
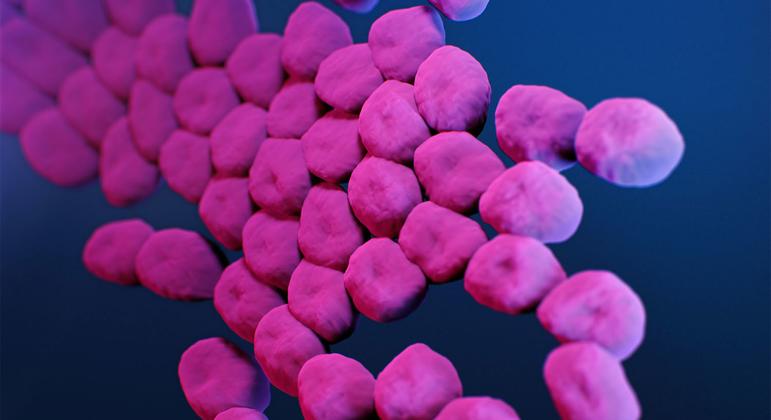
Antimicrobial resistance threatens the prevention and treatment of an increasing range of infections caused by bacteria, fungi, parasites and viruses.
It occurs when these bacteria, fungi, parasites, and viruses change over time and no longer respond to medications, making infections more difficult to treat and increasing the risk of disease spread, serious illness, and death. As a result, medications become ineffective and infections persist in the body, increasing the risk of infecting others.
Antimicrobials (including antibiotics, antivirals, antifungals, and antiparasitics) are medicines used to prevent and treat infections in humans, animals, and plants. Microorganisms that develop resistance to antimicrobials are sometimes called “superbugs.”